Myofascial pain syndrome is referring to irritation at the level of the muscles in your body, is basically a clinical description of chronic muscle pain.
Myofascial Pain Syndrome Facts & Information
Over 40 million Americans estimated to have this condition. This is usually found in head, neck, shoulders, extremities and back.
Pain is present locally and often referred to other parts of the body that arises from trigger points which are localized sensitive areas in the muscle that contain palpable, taut bands.
Most often it presents following an initial insult or trauma to deeper structures of the spine. The muscles respond by contracting around the injured area and in the low back is typically referred to as a low back strain. Initially, it is a subconscious protective reaction to decrease any activities that could potentially aggravate the pain. After some time, if the deeper injury does not improve and/or is not treated appropriately soon after the insult, the muscle spasms can serve to contribute to your overall pain.
Pain can be localized or widespread, often in conjunction with vague symptoms like numbness, fatigue, or sleep disturbance.
Our board-certified pain management doctor can accurately diagnose if MPS is the source of your pain and help you gain relief with highly effective non-surgical treatment.
How MPS generate pain?
This muscle tightness can be felt as “little knots” in the muscles of your spine. As the muscle tightens, it decreases the blood flow going to that muscle. Decreasing the blood flow leads to further muscle tightening from lack of oxygen to that muscle. This becomes a vicious cycle that can further increase your pain. Often these knots are very sensitive to even light pressure, these trigger points typically generate pain not only at the site, but also in various other areas of the body (referred pain).
You may experience symptoms that appear totally unrelated to the original injury.
MPS usually develops between ages 20 to 40 and is more common in women and people with less active lifestyles. 
After full evaluation that entails a detailed history and examination, the causes of MPS can be pin pointed.
Common underlying causes that can result in developing MPS:
- Damage to musculoskeletal tissues from trauma
- Previous neck or back surgeries
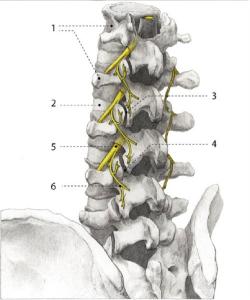
- Facet Joints Syndrome
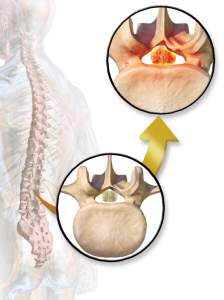
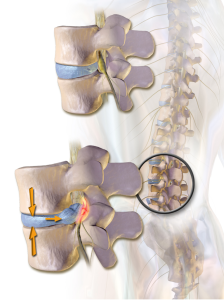
- Injured or herniated discs
- Wrong office seating ergonomics
- Heavy and wrong lifting mechanics
- Unconditioned muscles
- Prolonged Immobilization of a joint or a muscle group
- Fibromyalgia
- Medical conditions such as heart attack, stomach irritation, or gall bladder problems
- Electrolytes imbalance and/or Nutritional deficiencies (e.g. Chronic Kidney Conditions)
- Hormonal changes (PMS or menopause)
- Prolonged exposure to cold, such as sleeping in front of an air conditioning vent
Symptoms
- Headaches
- Neck Pain
- Jaw pain
- Low back pain
- Arm and leg pain
- Depression, fatigue, anxiety, or mood disturbances
Diagnosis & Treatments:
Proper diagnosis starts with an experienced pain management doctor. The type of pain that you may have with myofascial pain syndrome can be similar to the symptoms of several types of disorders.
Determining the correct source of your pain is critical to successful treatment – diagnostic procedures include:
- Begins with a thorough clinical evaluation
- Including a complete medical history, analysis of your symptoms, and physical examination
- Testing may include x-rays, MRI and/or CT scans, and electro-diagnosis (EMG)
Specific therapy directed at the underlying cause of your pain beyond the level of the muscles is the most important step to alleviate your pain. Once the specific cause of your pain is treated, the muscle spasms typically improve.
In the meanwhile, Anti-inflammatories and possibly Muscle Relaxants can be helpful in treating your spasms. These are not targeted at treating anything specifically but may help with the pain until your body heals.
Physical therapy is recommended as this can improve your spasms utilizing different treatment modalities including: heat, ultrasound, massage, electrical stimulation, dry needling etc. But this will bring us back to your inability to do any PT exercises because of your pain. That is why breaking this vicious circle by treating the underlying cause of the muscle spasms is crucial for a long term outcome.
If it is determined that the muscles are your primary pain generator, then Trigger Point Injections may help alleviate some of your symptoms. This involves injecting a mixture of medications into the muscles themselves to decrease the spasm and improve blood flow. Steroids are not typically recommended in treating muscle spasms.
As with all disease states, it is best to treat this early and aggressively as pain has memory and the longer you continue to have the pain, the more difficult it will be for your body to erase this memory.




![By James Heilman, MD (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](/assets/components/phpthumbof/cache/vcfrac3.25c355a85cb0101f004729be8d39bec3199.jpg)