Basic Facts & Information About Lumbar Spinal Stenosis
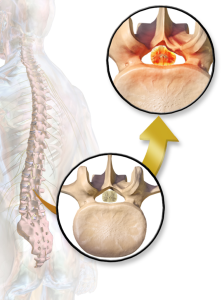
- A common cause of low back and leg pain, it literally means narrowing (Stenosis) of the Lumbar spine. As we age, our spines change. These normal wear-and-tear effects of aging can lead to narrowing of the spinal canal and this condition is called Spinal Stenosis.
- Lumbar spinal stenosis affects over 1.2 million people in the U.S. Degenerative changes of the spine are seen in up to 95% of people by the age of 50. Spinal stenosis most often occurs in adults over 60 years old. Pressure on the nerve roots is equally common in men and women.
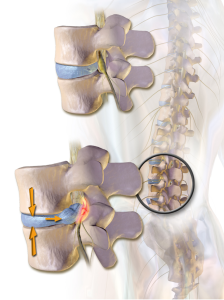
- Spinal stenosis occurs when the space around the spinal cord narrows. This puts pressure on the spinal cord and the spinal nerve roots, and patient may experience back pain that may radiate down one or both legs with associated weakness, numbness and tingling.
- Some people may not experience any pain but feels their legs are “heavy” or “rubbery” that is usually worse with standing and walking and gets better by sitting, resting, leaning forward and bending - like on a shopping cart.
- Spinal stenosis is not something that happens overnight.
What Causes Lumbar Spinal Stenosis
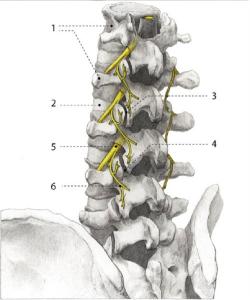
The condition typically involves Three factors in your spine that combine to cause the narrowing, they include:
- Disc problem usually a bulge that begins to push on the nerves from the front of your spine.
- Joints in your back that become enlarged secondary to arthritis (Lumbar Spondylosis) that pushes the nerves from the back of your spine.
- Thick Ligament that can becomes enlarged and also pushes from the back of your spine.
** At times, there also may be a slight misalignment of your spine that can contribute to the narrowing as well - Spondylolisthesis. 
These 3 factors continue to crowd the nerves in your low back but you usually do not experience any of the above symptoms until the narrowing reaches a critical level. Think of your spinal nerves as very bad neighbors. As they get too close to each other, they become aggravated and inflamed thereby producing symptoms.
Arthritis is the most common cause of Spinal Stenosis.
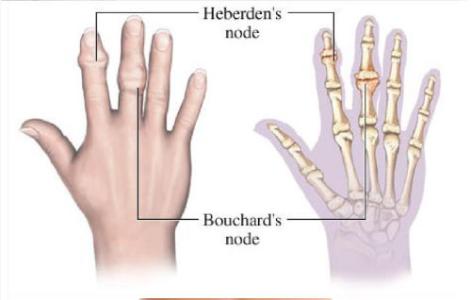
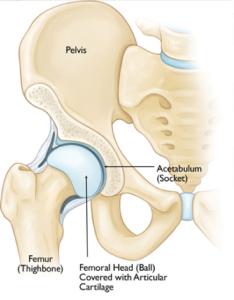
Arthritis refers to degeneration of any joint in the body. As the spine settles, two things occur. First, weight is transferred to the facet joints. Second, the tunnels that the nerves exit through become smaller.
As the facet joints experience increased pressure, they also begin to degenerate and develop arthritis, similar to that occurring in the hip or knee joint. The cartilage that covers and protects the joints wears away. If the cartilage wears away completely, it can result in bone rubbing on bone. To make up for the lost cartilage, your body may respond by growing new bone in your facet joints to help support the vertebrae. Over time, this bone overgrowth-called spurs-may narrow the space for the nerves to pass through.
Common Presentations To Lumbar Spinal Stenosis
Pain, Weakness, Heaviness
Most people with spinal stenosis can only walk for very short distance before the pain and/or weakness/heaviness causes them to rest. Some will find relief leaning forward often referred to as the shopping cart sign as leaning forward on a shopping cart will improve your symptoms. This opens the area of the narrowing of your spine to a small degree but can alleviate your symptoms.
Spinal Stenosis occurs through normal aging of the spine when nerves become crowded or compressed in the center of your spine, BUT it can be easily confused with other conditions in your spine that can cause similar symptoms.
Radicular Pain:
Nerves roots coming out of your spinal cord can also be pinched as they leave the spine as well. This will usually produce symptoms down one leg - Lumbar Radiculopathy- Vs Spinal Stenosis that typically involves both legs since the problem level is deeper, and before the nerves leave the spine.
Effective treatment plan always starts with accurate diagnosis, it is extremely important to differentiate which one or both diseases are causing your symptoms.
Both conditions may be seen on diagnostic studies, such as x-rays and/or MRIs, this does not necessarily mean they are both causing your symptoms. In addition, other conditions that may not be even related to your spine, such as narrowing of the blood vessels to your legs, may produce similar symptoms.
Being evaluated by experienced Spine Specialist is crucial in identifying a specific diagnosis who may order studies to support the clinical diagnosis.
Treatment Options:
Choosing the best treatment plan for you depends on multiple factors, like: How bad is your symptoms? Our goals/expectations for the treatment?
Typically there are either Surgical or Non-Surgical options.
I always encourage my patients to consider the less invasive, non surgical options first. This is important, specially with knowing that very high percentage of patients resume their life normally following accurate diagnosis and proper treatment early in the condition.
- Medications:
This certainly can give you some relief along with Physical Therapy, allowing you to continue to function but as the underlying condition is a chronic problem, this does not cure the underlying disease. In addition, like all medications, you must be careful in the side effects they may produce themselves and/or from the interactions they have with your current medication regimen. - Epidural Steroid Injection:
If medication management did not get you back into your normal life style and activity levels, you may be a candidate for Epidural Steroid Injections. Steroids are powerful anti-inflammatory class of drugs. This can help decrease the inflammation around the nerves that are causing your symptoms. Typically several of these are required to give you the relief you need. Most people can have months to years of relief from only this injections, while few others will have no relief. It is important that the steroid injection to be done accurately at the level where the stenosis is worst. - Minimally Invasive Surgeries:
If the above conservative less invasive measures fail or did not result in a long term pain relief outcome, minimally invasive surgeries might be an option to consider.
- One type of surgery that patients are encouraged to highly consider before considering more invasive surgeries, is called Spinal Cord Stimulator Trial. The good thing about this procedure that it gives you a chance to try it first, and that is why it is called a “Trial”. SCS trial lead placement, is as simple as an Epidural Injection, the only difference is that it is done under different sterile preparation that takes most of the procedure time…..for more information
After exhausting all the relatively less invasive approaches, if there is no improvement and the condition is not under control. Then we should be getting a Neurosurgical opinion for more invasive surgical options if you are a candidate for it.
As part of MAPMSC promise to our patients, we will work only as our patients’ advocate. We will only refer you to one of our collaborating trusted surgery team members, that we do recommend because we know they will give you the honest opinion that is only for your best interest. I always promise my patients that - I will only refer you to the same person I would refer one of my family members to.
The newer surgeries that you might be a candidate for, that you will get a chance to talk about in more details during your visit with the the neurosurgery team, are:
Interspinous Process Devices
Interspinous process devices, or spacers, are inserted between the spinous processes in the back of the spine. These devices spread the vertebrae apart and keep the space for the nerves open and functioning. This procedure is a minimally invasive surgical option for lumbar spinal stenosis.
Interspinous process spacers were approved in 2005. Many procedures have been performed since then. In some studies, success rates are greater than 80 percent.
Numerous spacer devices are currently being evaluated. They may be a safe alternative to an open laminectomy for some patients. Limited bone (lamina) is removed with this procedure, and it may be performed under local anesthesia.
The key to success with this procedure is appropriate selection of the patients. The appropriate candidate must have relief of buttock and leg pain when sitting or bending forward. The pain returns upon standing.
Minimally Invasive Decompression
Decompression can be performed using smaller incisions. When using such minimally invasive techniques, there is less injury to the surrounding soft tissues, and recovery may be quicker.
With these minimally invasive techniques, surgeons rely more on microscopes to see the area for surgery. They may also take X-rays during the operation. A traditional open procedure requires more direct visualization of the patient's anatomy, and therefore requires a larger incision. This can be more painful for the patient.
The limitation of minimally invasive surgery is the degree of visualization available. If the spinal stenosis extends over a large area of the spine, an open technique is the only method that can address the problem.
The advantages of minimally invasive procedures include reduced hospital stays and recovery periods. However, both open and minimally invasive techniques relieve stenosis symptoms equally. Your doctor will be able to discuss with you the options that best meet your healthcare needs.



![By James Heilman, MD (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](/assets/components/phpthumbof/cache/vcfrac3.25c355a85cb0101f004729be8d39bec3185.jpg)